Seborrheic dermatitis
Seborrheic dermatitis is a common skin and scalp disease that presents as red plaques covered with white or yellowish dandruff on areas where the skin and scalp are oily. It is a benign condition that is not serious but can be embarrassing, highly visible and may have a significant impact on the quality of life of those who suffer from it. This thematic guide aims to answer the questions you frequently ask yourself about seborrheic dermatitis, how to recognize it, how to fight it on a daily basis and how to learn to live better with it.
What is seborrheic dermatitis?
Seborrheic dermatitis is a chronic inflammatory dermatosis that can affect the skin, scalp or both. It presents as poorly defined erythematous plaques covered with small, non-sticky scales, of varying degrees of greasiness. On the scalp, it is characterized by intense itching and may be accompanied by a burning sensation.
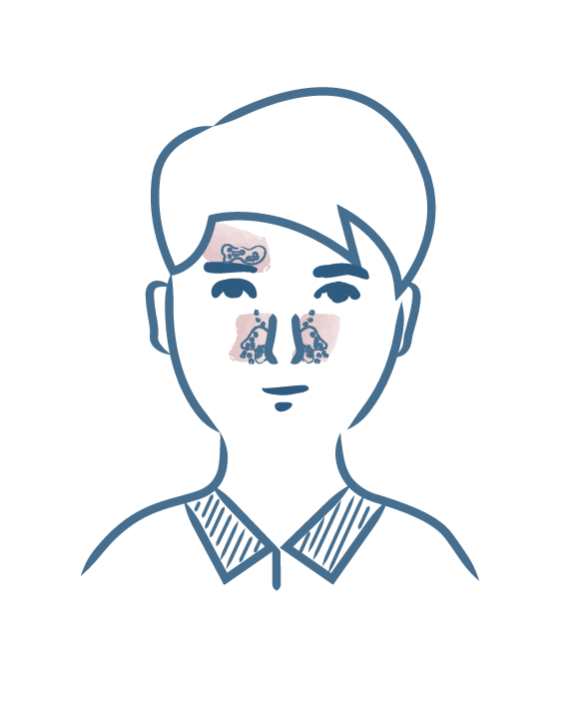
Lesions develop in the oily areas of the skin, where sebum secretion is greatest; such as the scalp, the furrow between the nose and cheeks, but also the eyebrows and the space between them, and the torso.
A physician can diagnose the disease based solely on the disease's visible manifestations. Nevertheless, some lesions may be similar to psoriasis, which sometimes makes it difficult to distinguish between the two conditions.
When the scalp is affected, scales can be mistaken for dandruff.
In the case of infants, we refer to cradle cap, which usually appear before the age of three months. It is recommended to use specific products adapted to treat cradle cap in infants.
Seborrheic dermatitis is not a serious disease, and therefore does not cause any complications. However, it can be esthetically embarrassing. In some patients, the disease may have a major impact on quality of life due to its recurrent nature.
Seborrheic dermatitis is a non-contagious disease, progressing in flare-ups, and can last several years. It is a common condition, mainly concerning teenagers and adults, and affecting up to 3% of the French population.
It is essential to clearly understand the nature of seborrheic dermatitis and to know how to tell it apart from other diseases.
What are the causes of seborrheic dermatitis?
At present, the causes of seborrheic dermatitis are still not known with certainty. However, three elements have been identified: sebum, which when in excess causes a yeast to proliferate,which itself induces inflammation. Sebum is naturally present on the surface of the skin in the so-called oily areas. In people suffering from seborrheic dermatitis, sebum is in excess and causes an abnormal proliferation of a yeast, also naturally present on the surface of the skin, called Malassezia. This yeast is responsible for the red plaques the condition causes. It triggers a specific inflammatory reaction, resulting in redness, and an accelerated renewal of scalp and skin cells, causing small white or yellowish scales on the skin surface.
Seborrheic dermatitis can be triggered by many factors, including:
- Climatic factors: humidity and cold, winter, perspiration
- Alcohol and tobacco consumption
- Periods of stress and fatigue
What is the best treatment for seborrheic dermatitis?
At present, there is no therapeutic treatment that can definitively cure seborrheic dermatitis. However, it is nevertheless possible to act effectively on symptoms and to reduce the frequency of recurrence as far as possible.
Topical treatments in the form of medicinal treatments or dermo-cosmetic products are recommended for seborrheic dermatitis.
In some severe cases, physicians may use oral treatments, but this is exceptional.
Treatment is effective but only acts on symptoms. Symptoms may therefore reappear during a new flare-up or when treatment is stopped prematurely. Treatment consists of reducing seborrhea and the colonization of Malassezia-type yeast, and thus inflammation, from the first signs.
The proposed treatment may vary according to the affected areas and the evolution of the disease.
Living with seborrheic dermatitis on a daily basis
A few basic daily rules can help fight seborrheic dermatitis and prevent or delay the onset of a new flare-up by reducing the promoting factors as far as possible:
- Ensure good skin and scalp hygiene using gentle dermo-cosmetic products adapted to the condition.
- In order to avoid further irritation and to prevent reactivation of the inflammatory circle, dry the skin by patting without rubbing when washing and avoid scratching the lesions as far as possible.
- Pay special attention to your skin in case of fatigue or overwork.
- Adopt a healthy and balanced diet.
- Reduce alcohol and tobacco consumption as much as you can.
- Make the most of the sun while protecting yourself.
The treatment of seborrheic dermatitis symptoms is highly effective. In case of doubt or difficulties in complying with your treatment, do not hesitate to consult your dermatologist, your general practitioner or your pharmacist to find suitable solutions with them.
Our care routines
Irritated skin with redness and scales